Malaysia is once again on high alert for malaria due to increase in number of cases and detection of a new malaria parasite in three villages in the town of Kuching, Sarawak. The newly discovered malaria parasite is identified as Plasmodium knowlesii, which is transmitted from infected monkeys to Anopheles mosquitoes which is then passed down to humans.
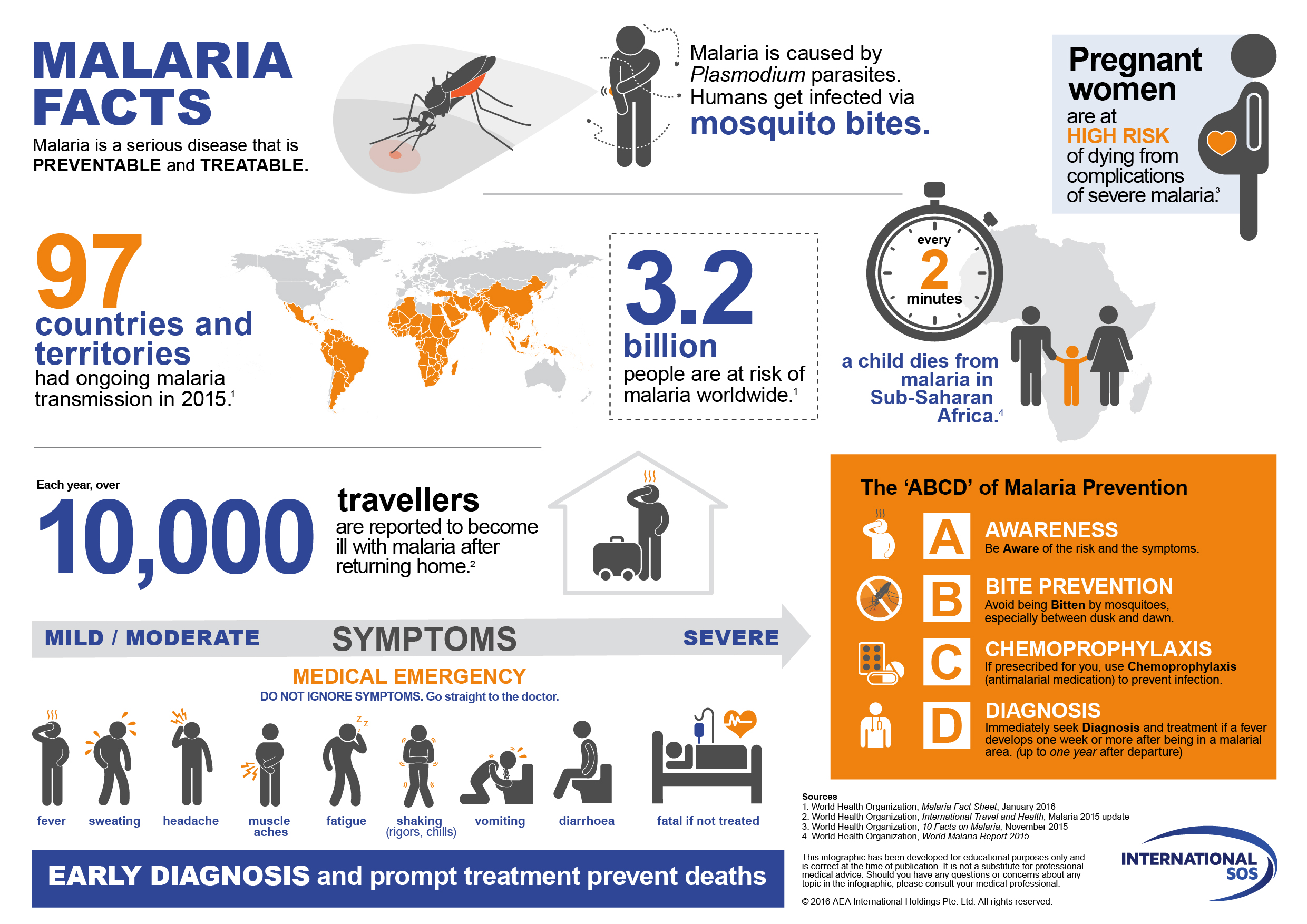
What is Malaria? Malaria, primarily found in South Asia and sub-Saharan Africa, is a life-threatening disease caused by parasites. There are five known malaria parasite species, and two of them – Plasmodium falciparum and Plasmodium vivax – pose the greatest threat. These parasites are transmitted to humans by the bite of an infected female Anopheles mosquito.
| When bitten by an infected Anopheles mosquito, the parasites are released into the bloodstream. The parasites travel through blood to the liver, where they mature. They then re-enter into the bloodstream and begin to infect red blood cells causing the typical symptoms of malaria. |
Symptoms of Malaria Depending on the species of Plasmodium a person has been invaded with, the time from the initial mosquito bite until symptoms appear can range from seven days to about a month. This is the incubation period. Severity of the symptoms also depends on the species as well as the individual’s general health.
Typical initial symptoms include fever, headache, chills and vomiting, they may be mild and vague, hence the difficulty to recognise malaria early. Symptoms then come and go in cycles. The time interval between episodes of fever and chills varies from 24 to 72 hours among the five species. Some species may cause more serious complications, such as damage to the heart, lungs, kidneys, or brain, and can be deadly.
| Some population groups are at considerably higher risk of contracting malaria, and developing severe disease, than others. These include infants, children under 5 years of age, pregnant women patients with HIV/AIDS, non-immuned migrants, mobile populations and travellers. |
Diagnosis of Malaria Early and accurate diagnosis of malaria is essential to ensure quick and effective disease management as well as rapid surveillance to prevent spread of infection in the community via local mosquitoes. The flu-like symptoms of malaria sometimes makes it difficult to detect. Malaria can be suspected based on the person’s travel history to endemic countries, symptoms, and the physical examination findings. 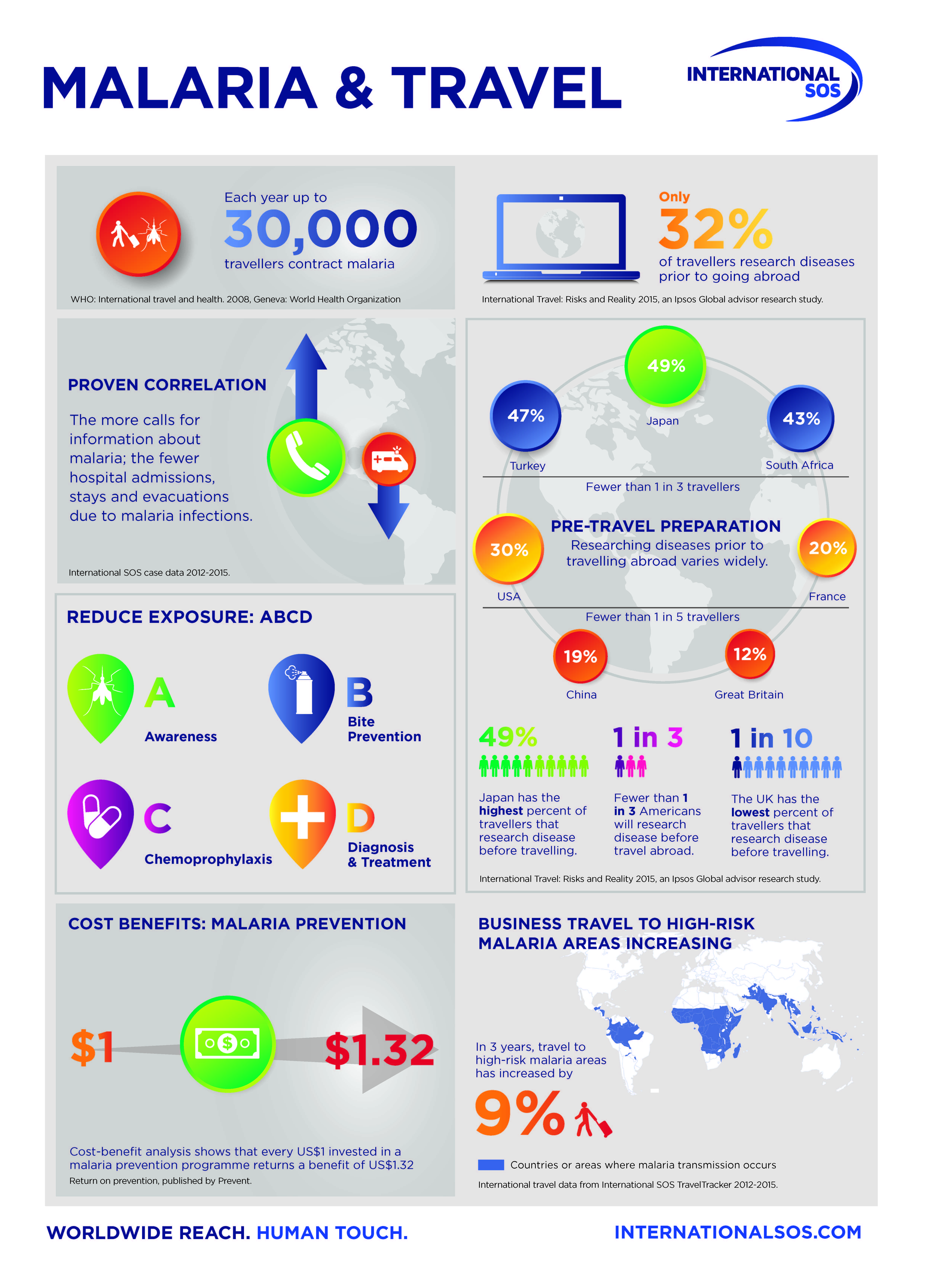 For a definitive diagnosis to be made, laboratory blood smear tests must demonstrate the presence of malaria parasites or their components. The blood test is also performed to monitor cure and relapses, and to determine drug susceptibility of the parasite causing the infection. When lab test is not readily available, rapid diagnostic tests sometimes called “dipstick” tests may be used instead. These tests detect malaria antigens (proteins) in a sample of a person’s blood, usually taken with a “fingerstick”. A colour change on the testing strip indicate a positive result. Delay in diagnosis and treatment is the leading cause of death in malaria patients. Treatment and Prevention Fortunately, malaria is treatable and preventable, and increased efforts globally are dramatically reducing the malaria burden in many places. According to UNICEF, over the last 15 years, the delivery of core malaria interventions has undergone an unprecedented expansion. For example, since 2000, one billion insecticide-treated mosquito nets have been distributed in Africa. These bed nets are not only an effective means of preventing malaria by creating a protective barrier against mosquitoes at night, but also simple and cost-friendly. The introduction of rapid diagnostic tests has made it possible to distinguish between malarial and non-malarial fevers more quickly – enabling timely appropriate treatment. Artemisinin-based combination therapies (ACTs) are highly effective against Plasmodium falciparum, the most prevalent and lethal malaria parasite. A full course of life-saving malaria treatment costs is just USD1 and cures a child in one to three days.
For a definitive diagnosis to be made, laboratory blood smear tests must demonstrate the presence of malaria parasites or their components. The blood test is also performed to monitor cure and relapses, and to determine drug susceptibility of the parasite causing the infection. When lab test is not readily available, rapid diagnostic tests sometimes called “dipstick” tests may be used instead. These tests detect malaria antigens (proteins) in a sample of a person’s blood, usually taken with a “fingerstick”. A colour change on the testing strip indicate a positive result. Delay in diagnosis and treatment is the leading cause of death in malaria patients. Treatment and Prevention Fortunately, malaria is treatable and preventable, and increased efforts globally are dramatically reducing the malaria burden in many places. According to UNICEF, over the last 15 years, the delivery of core malaria interventions has undergone an unprecedented expansion. For example, since 2000, one billion insecticide-treated mosquito nets have been distributed in Africa. These bed nets are not only an effective means of preventing malaria by creating a protective barrier against mosquitoes at night, but also simple and cost-friendly. The introduction of rapid diagnostic tests has made it possible to distinguish between malarial and non-malarial fevers more quickly – enabling timely appropriate treatment. Artemisinin-based combination therapies (ACTs) are highly effective against Plasmodium falciparum, the most prevalent and lethal malaria parasite. A full course of life-saving malaria treatment costs is just USD1 and cures a child in one to three days.
| Malaria may become a medical emergency without prompt and appropriate treatment as the biggest challenges are related to growing drug and insecticide resistance. WHO official reported that mosquito resistance to insecticide and anti-malarial drugs have been an increasing concern. It is therefore crucial to increase research funding as countries need to stay ahead of the development of drug resistance. |
For example since 2010, 60 of the 73 countries that monitor insecticide resistance have reported mosquito resistance to at least one type of insecticide used in nets and indoors sprays. A silver lining was when WHO recently announced that the world’s first malaria vaccine would be rolled out through pilot projects in three sub-Saharan African countries in 2018. If the vaccine trial is a success, the drug would be widely distributed across the globe. The control and eradication of malaria demands many-sided approach. As World Health Organisation initiatives reach more communities and people at risk for malaria, many more lives will be saved.
| Malaysia has come a long way in the prevention and control of malaria since the introduction of the Malaria Eradication Programme in 1960. At present Malaysia has a range of good tools, including insecticide spraying and public health awareness campaigns. But no preventative strategy is 100% effective – there will always be cases that slip through the net. While scientists and organisations around the world are working together to accelerate the development of a malaria vaccine and ensure its availability in the developing world, fighting malaria is the responsibility of the community as a whole. |
We have the tools to put an end to it, and prevention is better than cure. Let’s make malaria no more! Malaria Pocket Guide This article is brought to you by IMU Healthcare. References 1. Management Guidelines of Malaria in Malaysia. Ministry of Health Malaysia 2016. 2. https://www.cdc.gov/malaria/diagnosis_treatment/diagnosis.html 3. https://sg.news.yahoo.com/sarawak-alert-malaria-bug-found-110600596.html 4. http://www.who.int/malaria/en/ 5. http://www.mmv.org/malaria-medicines/malaria-treatment 6. http://www.who.int/mediacentre/factsheets/fs094/en/ 7. https://s-media-cache-ak0.pinimg.com/originals/fc/7c/c2/fc7cc2ca91316a8cca86cedef8d56e64.jpg 8. http://www.theborneopost.com/2016/12/07/dr-jerip-foreign-workers-with-communicable-diseases-will-be-deported/ 9. https://www.unicef.org/health/index_malaria.html 10. https://www.internationalsos.com/topics/malaria2016