Schizophrenia is categorised as a severe mental disorder which results in changes in behavior, thinking, memory, speech, thought and even movements. These changes result in significant changes in an individual’s capacity to function both in social and occupational spheres. Unfortunately, the disease usually begins in late adolescence and early adulthood, during the most critical phase of an individual’s life cycle. This is the phase during which individuals complete their secondary or tertiary education, get employment, form relationships, get married and start families. Thus, schizophrenia results in a huge cumulative loss to society as a whole. IMU Healthcare Neuro-Psychiatrist, Dr Shane Varman, shares how depressive symptoms have been recognised to coexist with schizophrenia. This is to be expected considering the impact the illness has on the individual. The prevalence of depression among schizophrenics has been reported to vary between 60 % in newly diagnosed patients and 50% in the more chronic patients.
SCHIZOPHRENIA – SYMPTOMS
How Does the Presence of Depression Impact Individuals with Schizophrenia? Individuals usually progress through a ‘prodromal phase’ of illness before the first episode of Schizophrenia occurs. During this prodromal phase, individuals experience low self-esteem, disturbed sense of self, disturbed self-image and begin to experience transient hallucinations and suspiciousness. Depression and anxiety, says Dr Shane, begins at this phase. Depression which is compounded by low self-esteem and disturbed self-image, may even lead to suicidal thoughts and attempt. Anxiety symptoms often manifest as social-anxiety. This social anxiety worsens the social withdrawal. Keeping in mind that these symptoms have started before the actual acute phase of the illness begins, one can empathise with the sufferers. Withdrawn from family and friends, individuals start to abuse drugs as means of coping with a myriad of symptoms. During the acute phase of Schizophrenia, florid hallucinations and delusions torment and terrorise the individual. With their perceptions, senses and sense of reality taken over by the illness, patients are confused, frightened and have lost the ability to reason or make sense of what’s happening to them. Depressive symptoms are present and hallucinations command the individual to harm him or herself. It’s during this phase that most families succeed in bringing the individual to the hospital, and the investigative and diagnostic process begins. After the usually successful treatment with anti-psychotic medication, individuals are allowed home to recover. Post-discharge phase; it’s during this phase which individuals are at highest risk of suicide. “Having been told that they suffer from Schizophrenia, individuals are devastated and understandably depressed”, shares Dr Shane. With a myriad of blogs providing wrong information of the illness, individuals and family members can be misguided into stopping medication and follow-ups prematurely. Visits to alternative healers, if have not taken place, will ensue. Alternative therapies have found to be helpful in most societies, provided medications and follow-ups are adhered to. Alternative healers often provide an ’acceptable model’ of the illness. Thus, it’s easier for patients and family members to accept cultural models of mental illness, i.e. that if it’s caused by a ‘djin’ or ‘black-magic’. Many traditional healers in Malaysia actually encourage individuals to continue with their anti-psychotic medication. However, there are the unscrupulous few who manipulate and financially drain families who are already in dire straits. During the chronic phase of the illness, individuals with schizophrenia begin to manifest the negative symptoms of the illness. During which there is loss of motivation, self-neglect from apathy, emptiness of thought and continued social withdrawal. They have to deal with stigma, where they are or feel ostracised by the community. They can’t earn an income which leads to further loss of self-esteem. Social withdrawal aggravates the stigma. Depression during the chronic phase is often unrecognized or explained as ‘chronic symptoms’ of Schizophrenia. Suicide attempts can occur during this period as well.
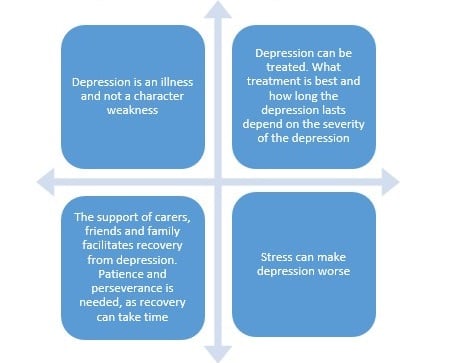
DEPRESSION: WHAT YOU NEED TO KNOW
http://www.who.int/campaigns/world-health-day/2017/handouts-depression/someone-with-depression/en/
 How Can Schizophrenia be Treated? Treatment is multi-dimensional. A psychosocial assessment is done and antipsychotic medications are prescribed, if schizophrenia is confirmed. These medications, if taken as prescribed, are not only effective but crucial to remove all auditory hallucinations and resolve the psychosis. Psychosocial and occupational therapy would be needed as well to help patients become functional again. Simple day to day activities are monitored to ensure that self-care is not neglected. Dr Shane cautions that, “Symptoms such as low motivation and social withdrawal are harder to treat. Patients with severe depression may be prescribed with antidepressants to help them cope. If depression is not treated, suicidal tendencies are definitely a concern.” Will Schizophrenia Patients Live a Normal Life Again? This is a chronic illness which means continued treatment and support are needed. Generally, statistics show that about 20-30% can go back to work in a sheltered environment whereby employers are aware of their disability and make allowances for their needs such as going back for hospital admissions. Many Malaysians are compassionate and employ people with this illness. Similarly, many schools and universities are very supportive in giving counselling and encouragement to help their students cope with treatment and their depression. Students are allowed to complete a course within their abilities or to opt for courses with a lighter workload. What Can Family Members Do To Help? It is important that they learn to do it the right way. Psychiatrists and psychotherapists can advise family members of how they can help the patients cope in their daily lives. Patients tend to feel depressed, hence, being over-involved and over-protective might stress them out. On the other hand, do not neglect the patient. Find a balanced way to help and care. Many major hospitals have support groups for family members as there is a learning curve in dealing with this illness. How Can Schizophrenia Be Prevented? Dr Shane recommends that people with a family history of schizophrenia, as well as other mental illness, take steps to lower their risk by practicing a healthy lifestyle and having a positive outlook on life. Reduce mental stress by optimising your diet, having proper exercise, being disciplined and avoid taking any substances. Maintain a healthy family and have good relationships with family members where anyone can express feelings, share personal problems, and find solutions. Meditation, yoga, mindfulness and other stress-reduction techniques are often described as recent discoveries but are actually age-old Eastern methods of coping with stress. For people diagnosed with schizophrenia, Dr Shane advocates that, “with proper treatment and continued support, they can return to normal function in sheltered environments. It is good to be hopeful. There are many types of assistance available including training for jobs.” Our care and compassion can certainly encourage people with schizophrenia to be functional members of the community. Always lend a listening ear and have empathy for them so that they know that life is still worth living. References: 1. http://www.iku.gov.my/images/IKU/Document/REPORT/nhmsreport2015vol2.pdf 2. http://www.who.int/mental_health/management/schizophrenia/en/ 3. Upthegrove R, Marwaha S, Birchwood M. Depression and Schizophrenia: Cause, Consequence or Trans-diagnostic Issue? Schizophr Bull. 2016 Jul 15. pii: sbw097. 4. Haug E, Øie MG, Andreassen OA, Bratlien U, Romm KL, Møller P and Melle I(2016) The association between anomalous self-experiences, self-esteem and depression in first episode schizophrenia. Front. Hum. Neurosci. 10:557. doi:10.3389/fnhum.2016.00557 This article is brought to you by IMU Healthcare.
How Can Schizophrenia be Treated? Treatment is multi-dimensional. A psychosocial assessment is done and antipsychotic medications are prescribed, if schizophrenia is confirmed. These medications, if taken as prescribed, are not only effective but crucial to remove all auditory hallucinations and resolve the psychosis. Psychosocial and occupational therapy would be needed as well to help patients become functional again. Simple day to day activities are monitored to ensure that self-care is not neglected. Dr Shane cautions that, “Symptoms such as low motivation and social withdrawal are harder to treat. Patients with severe depression may be prescribed with antidepressants to help them cope. If depression is not treated, suicidal tendencies are definitely a concern.” Will Schizophrenia Patients Live a Normal Life Again? This is a chronic illness which means continued treatment and support are needed. Generally, statistics show that about 20-30% can go back to work in a sheltered environment whereby employers are aware of their disability and make allowances for their needs such as going back for hospital admissions. Many Malaysians are compassionate and employ people with this illness. Similarly, many schools and universities are very supportive in giving counselling and encouragement to help their students cope with treatment and their depression. Students are allowed to complete a course within their abilities or to opt for courses with a lighter workload. What Can Family Members Do To Help? It is important that they learn to do it the right way. Psychiatrists and psychotherapists can advise family members of how they can help the patients cope in their daily lives. Patients tend to feel depressed, hence, being over-involved and over-protective might stress them out. On the other hand, do not neglect the patient. Find a balanced way to help and care. Many major hospitals have support groups for family members as there is a learning curve in dealing with this illness. How Can Schizophrenia Be Prevented? Dr Shane recommends that people with a family history of schizophrenia, as well as other mental illness, take steps to lower their risk by practicing a healthy lifestyle and having a positive outlook on life. Reduce mental stress by optimising your diet, having proper exercise, being disciplined and avoid taking any substances. Maintain a healthy family and have good relationships with family members where anyone can express feelings, share personal problems, and find solutions. Meditation, yoga, mindfulness and other stress-reduction techniques are often described as recent discoveries but are actually age-old Eastern methods of coping with stress. For people diagnosed with schizophrenia, Dr Shane advocates that, “with proper treatment and continued support, they can return to normal function in sheltered environments. It is good to be hopeful. There are many types of assistance available including training for jobs.” Our care and compassion can certainly encourage people with schizophrenia to be functional members of the community. Always lend a listening ear and have empathy for them so that they know that life is still worth living. References: 1. http://www.iku.gov.my/images/IKU/Document/REPORT/nhmsreport2015vol2.pdf 2. http://www.who.int/mental_health/management/schizophrenia/en/ 3. Upthegrove R, Marwaha S, Birchwood M. Depression and Schizophrenia: Cause, Consequence or Trans-diagnostic Issue? Schizophr Bull. 2016 Jul 15. pii: sbw097. 4. Haug E, Øie MG, Andreassen OA, Bratlien U, Romm KL, Møller P and Melle I(2016) The association between anomalous self-experiences, self-esteem and depression in first episode schizophrenia. Front. Hum. Neurosci. 10:557. doi:10.3389/fnhum.2016.00557 This article is brought to you by IMU Healthcare.