IMU Healthcare Consultant Obstetrics and Gynaecology, Dr Kavitha Nagandla highlights the importance of cervical cancer vaccination and screening for women.
| Human Papillomavirus and Related Diseases Report on Malaysia 2019 from the ICO/IARC Information Centre on HPV and Cancer |
|---|
| Cervical cancer ranks as the third leading cause of female cancer in Malaysia |
| Cervical cancer is the second most common female cancer in women aged 15 to 44 years |
| Approximately 1,682 new cervical cancer cases are diagnosed annually in Malaysia (estimates for 2018) . |
Human papillomavirus (HPV) infection is a well-established cause of cervical cancer and there is growing evidence of HPV being a relevant factor in other anogenital cancers (vulva, vagina, anus and penis) as well as head and neck cancers. “Any woman who is sexually active or used to be sexually active may be at risk of contracting cervical cancer,” says Dr Kavitha Nagandla, Consultant Obstetrics & Gynaecology at IMU Healthcare.
HPV refers to a group of more than 200 related viruses with over 40 types transmitted through direct sexual contact – vaginal, anal, and oral sex – from the skin and mucous membranes of infected people to those of their partners . Infections may be asymptomatic. However, prolonged and persistent infections with high-risk types can lead to cell changes that, if left untreated, may progress to cancer. Studies reveal that up to 88.7% of invasive cervical cancers are attributed to HPVs 16 and 18 . Early detection via screening and vaccination can reduce the risk of cancer by up to 70% . Cervical cancer is usually found in women who are in their 30s to 40s. To mitigate the risk of cervical cancer in the female population, the Ministry of Health Malaysia has since 2010 introduced through schools, the Human Papilloma Virus (HPV) vaccination programme for girls aged 13.
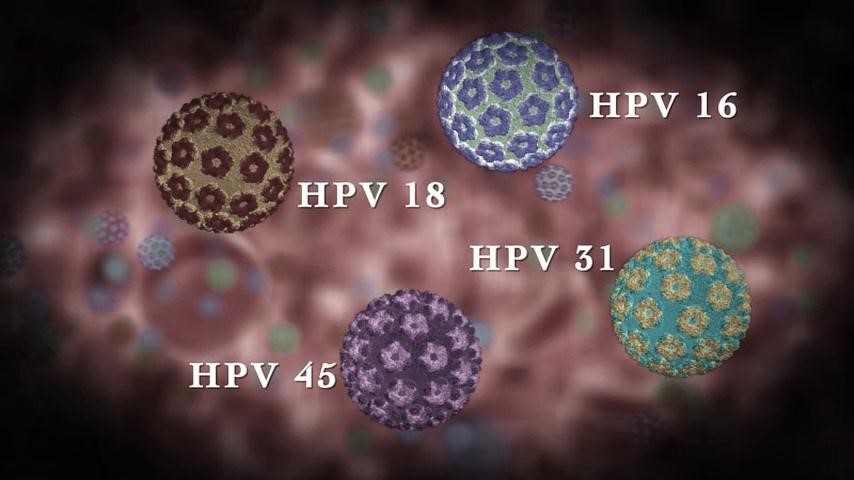
“The reason why pre-teen girls are vaccinated is because they are presumed to not have had any sexual contact at the age of 13,” says Dr Kavitha. HPV vaccines are highly effective in reducing the potential risk of infection for the types of HPV they target when given prior to initial exposure to the virus . When the vaccine is given, it stimulates the body to produce antibodies that, in future encounters with other HPVs, bind to the virus and prevent it from infecting cells thereby offering cross protection . “This is the rationale for HPV vaccination in older women as well, as it cross-protects against other viruses that can cause cancer should they be exposed to them in future. Hence, older women may not get 80-90% protection like school children but may get about 30% protection. Some cross protection is still beneficial,” says Dr. Kavitha. Currently, vaccination to prevent cervical cancer is available for individuals until the age of 45 and may be extended until the age of 50. In clarifying myths in relation to HPV and cervical cancer, Dr Kavitha says, “Cervical cancer does not run in the family like ovarian and uterine cancer. It is a lifestyle-related condition.” Individuals with multiple sexual partners and/or are exposed to sex at an early age run a higher risk of HPVs and cervical cancer . Dr Kavitha adds, “Contraception like The Pill or jabs will not protect an individual from cervical cancer, although condoms may offer some protection against HPV infection. HPV cannot live outside the body and be transmitted via fomites like tabletops and bedsheets as it requires a medium or cellular structure and nutrients for survival. The virus only infects at the cellular level and targets cells at the neck of the womb or cervix. Once minor surgery is done to remove the abnormal cells, the patient is potentially cured.” Another common misconception regarding cervical cancer relates to vaccination and screening. “Women need to understand that the vaccine does not offer 100% protection. It does not prevent other sexually transmitted diseases (STDs), nor does it treat existing HPV infections or HPV-caused diseases or protect against all HPV infections that cause cancer,” says Dr Kavitha. “Although the vaccine is very effective, we still need more data and until then, women regardless of whether or not they are vaccinated are strongly advised to undergo regular screening.”
“The purpose of screening is to catch abnormalities in the cells early so there can be early intervention,” says Dr Kavitha, adding that HPV not only causes cancer but also non-cancerous conditions like warts on the hands, feet, eye lids, lips and genital area but these conditions are highly treatable.
In identifying red flags with regards to cervical cancer, women in general should look out for signs and symptoms that includes abnormal bleeding between menstrual periods, post-coitus or post-menopause; discharge that is unusual in amount, consistency, color or smell; frequent or painful urination; and pelvic pain . “See your gynaecologist if you notice anything out of the ordinary,” says Dr Kavitha. A Pap Smear would usually be recommended by the specialist. Pap smear is a procedure in which a small brush or spatula is used to gently remove cells from the cervix to be checked for cell abnormalities that may lead to cervical cancer . It is essentially a test that detects pre-cancerous cells and is done as part of a pelvic exam. It is highly recommended to combine HPV DNA testing alongside the pap smear test .
An annual Pap smear coupled with HPV testing is important to ensure that both results are normal. In general, women aged 21-50 should get a Pap Smear done annually. If the results are normal 2 years in a row, then they should do it every 3 years. Women aged 50-65 should have it done every 5 years whilst women aged 65 and above should get checked if they have signs and symptoms ie; post-menopausal bleeding. Women who used to be sexually active should continue getting the Pap smear as they are still at risk of developing cervical cancer from past relationships. A Pap smear is not required for women who have never had any sexual intercourse as there is practically no risk of contracting HPVs nor cervical cancer. “If there is an option for HPV screening, we would advise the patient to do it as Pap Smear alone is not sufficient to identify potential issues with the cervix. Although Pap Smear is the most common form of screening for cervical cancer, its sensitivity is only 50%. That’s why doctors are now advocating that along with the Pap Smear, patients should also do HPV testing. It’s done in one shot and HPV testing is 99% sensitive so you will feel so much more assured. In US and currently UK, health authorities advocate doing only HPV screening as primary screening over Pap Smear,” says Dr Kavitha. “There needs to be more awareness on the HPV test and how it is a more accurate form of screening. The sensitivity is so high, you can repeat the HPV test every 5 years if confirmed negative,” she adds. Dr Kavitha continues: “If a patient’s Pap smear reveal the presence of cells that are slightly abnormal, we advise them not to smoke. Smoking and alcohol are high risk factors for women with some cell abnormality as it encourages the rogue cells to multiply. Smoking may lower one’s immunity to diseases so the virus that’s already present may cause abnormal cells to multiply faster.”
Cervical cancer is not only curable if detected early but is also largely preventable. With treatment and regular follow-ups with a gynaecologist, a woman with an abnormal smear result has a good chance of preventing the development of cervical cancer.
On whether a woman can still have child if she has cervical cancer, Dr Kavitha says, “In cases where the cancer is in its early stages and surgery is done to remove only abnormal cells in the cervix and the uterus is intact, there is a chance that the woman can become pregnant. However, she must be on follow up and that’s only in Stage 1. The moment it is above Stage 1, it becomes quite impossible because if you try to keep the womb intact, the cancer will spread.” Dr Kavitha hopes that with increased awareness, fewer women will be afflicted with this preventable disease resulting in a lower death rate from cervical cancer in Malaysia. “Pre-invasive disease of cervix which means abnormal pap smear and not cervical cancer yet is potentially curable. Cervical cancer is also treatable and curable if diagnosed in the early stages. The treatment can be highly effective. There is no similar screening for womb or ovarian cancer but for cervical cancer, vaccination and screening is available, there just needs to be more awareness for women to take the necessary preventive steps to ensure they stay in the pink of health.” Related article: Catching Cervical Cancer (The Star, 8 March 2020).