What is buccal cancer?
-Buccal cancer or mouth cancer is the cancer of the mouth. -The buccal mucosa is the lining of the cheeks and the back of the lips, inside the mouth where they touch the teeth. – It occurs more often in men, with a male:female ratio of 3-4:1, and most commonly in the 7th or 8th decade of life. – Incidence of buccal carcinoma is much higher in Asia, likely related to the widespread practice of tobacco and betel nut chewing – In Malaysia, the incidence is highest among the Indians, especially among females.
What are the risk factors of buccal cancer? – Smoking. Mouth cancer is just one cancer which has a much higher incidence in smokers than in non-smokers. – Alcohol. Drinking a lot of alcohol can increase your risk of developing mouth cancer. – Chewing tobacco or the betel leaf. – Poor dental hygiene. – Dietary factors (eating a well-balanced diet – high in fruits, vegetables and fish and low in high-fat and cholesterol meats, rice and refined grains – can reduce the risk of oral cancer). – The human papillomavirus (HPV) may increase your risk of mouth cancer.
What are the signs and symptoms? -Mouth sore that does not heal with medication -Mouth sore that bleeds spontaneously -Velvety white, red or speckled (white and red) patches in the mouth that are persistent -Hard, raised lesion (lump), crusts, eroded areas on the lips, gums or other areas inside the mouth -Unexplained bleeding in the mouth -Persistent pain in the mouth -Difficulty chewing, swallowing, speaking or moving the tongue -Loose teeth or dentures feeling unconfortable and not fitting properly -A change in your voice or speech problems How is buccal cancer diagnosed? A doctor will examine the inside of the mouth and back of the throat to check the location and size of the tumor. Examination of the ears, nose and neck are needed to help determine if the tumor has spread to the surrounding lymph nodes and other organs. The doctor may also order other tests including: – Blood tests – X-rays to determine if the tumor has spread to the lungs – Fine Needle Aspiration Biopsy (FNA). A thin needle is placed in the mouth. The cells are aspirated (suctioned) and then examined under a microscope to determine if the lump is cancerous – Imaging studies to determine if the tumor has invaded nearby tissues or other organs of the body. These may include: (i) Computerized tomography (CT) scan. A computer is linked to an X-ray machine which creates a series of detailed pictures, with different angles, of areas inside the mouth and neck. (ii) Magnetic resonance imaging (MRI). This machine uses a magnet, radio waves and a computer to create detailed pictures of the area inside the mouth and neck. (iii) Positron emission tomography (PET) scan. During a PET scan, a small amount of radioactive glucose (sugar) is injected into a vein. The scanner creates computerised pictures of the areas inside the body Staging of buccal cancer The TNM Classification of Malignant Tumours (TNM) is a cancer staging notation system that gives codes to describe the stage of a person’s cancer, when this originates with a solid tumor. -T describes the size of the original (primary) tumor and whether it has invaded nearby tissue, -N describes nearby (regional) lymph nodes that are involved, -M describes distant metastasis (spread of cancer from one part of the body to another). The aim of staging is to find out: -How much the tumour has grown in the mouth. -Whether the cancer has spread to local lymph nodes. -Whether the cancer has spread to other areas of the body (metastasised).
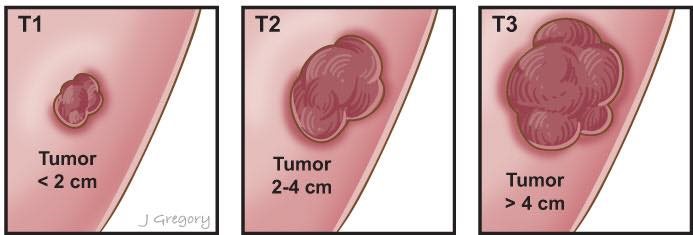 Figure 3. T-staging of the buccal cancer.
Figure 3. T-staging of the buccal cancer.
How is buccal cancer treated? Treatment options which may be considered include radiotherapy, surgery and chemotherapy. The treatment advised for each case usually depends on various factors such as the exact site, extent and spread of the cancer and your overall general health. (i) Surgery The most common treatment is surgery. The type of operation depends on the size of the cancer and its site. The operation may be to remove the cancer and some of the surrounding normal tissue. Sometimes surgery is aimed at curing the cancer by removing it all. Sometimes surgery is used to relieve symptoms if the cancer is at an advanced stage (palliative surgery). The operations are all done whilst you are asleep under a general anaesthetic. Laser surgery may sometimes be used to remove small mouth cancers. This may be combined with a light-sensitive medicine via treatment known as photodynamic therapy (PDT). (ii) Radiotherapy Radiotherapy is a treatment which uses high-energy beams of radiation which are focused on malignant (cancerous) tissue. This kills cancer cells, or stops cancer cells from multiplying. Two types of radiotherapy are used for mouth cancer: external and internal. -External radiotherapy. Radiation is targeted on the cancer, from a machine. (This is the common type of radiotherapy which is used for many types of cancers.) -Internal radiotherapy (brachytherapy). This treatment involves placing small radioactive wires next to the cancer for a short time and then they are removed. (iii) Chemotherapy Chemotherapy is a treatment which uses anti-cancer medicines to kill cancer cells, or to stop them from multiplying. Chemotherapy may be used in conjunction with radiotherapy or surgery. Chemotherapy may also be advised if the cancer has spread to other areas of the body. What is the prognosis after treatment? If a mouth cancer is diagnosed and treated at an early stage then there is a good chance of a cure. A cure is less likely if the cancer has spread. The treatment of cancer is a developing area of medicine. New treatments continue to be developed and the information on the outlook is very general. The specialist who knows your case can give more accurate information about your particular prognosis and how well your type and stage of cancer is likely to respond to treatment. Prepared by: A/Prof Rumi Khajotia, MD Ng Yang Jein, Semester 9, International Medical University Chai Yee Jy, Semester 9, International Medical University A/Prof Rumi Khajotia MBBS (Bom), MD (Bom), MD (Vienna), FAMA (Vienna), FAMS (Vienna) Associate Professor in Pulmonary and Internal Medicine, International Medical University, Malaysia Consultant Pulmonologist, Hospital Tuanku Ja’afar, Seremban, Malaysia A/Prof Rumi Khajotia is a Consultant Pulmonologist. His fields of interest include COPD, Bronchial Asthma and Lung Cancer. He has published a number of research articles and case studies in peer-reviewed international medical journals, on these subjects.











