Imagine this, you’re having a night out with your friends and everyone is having a good time chatting and laughing, but every time you laugh, you feel some urine leaking out. You know you only had two small glasses of water to drink in the past four hours, but yet you keep feeling the urge to run to the toilet each time the waiter pours water to refill glasses at the table. This condition is something that people who have urinary incontinence experience.
Urinary incontinence is at least twice as common in women as in men; with 30-60% of middle-aged to older women have some form of incontinence. In an 11-country study of Asian women, including Malaysia, the prevalence of urinary incontinence is found to be 53% with various symptoms. This includes sudden and intense urge to urinate, minor leaks, or frequent dribbling of urine.
Let’s dig deeper to find out more about this condition with Dr Sharifah Sulaiha Syed Aznal, a gynaecologist with special interest in urogynaecology at IMU Healthcare, and learn what we can do to prevent or manage it for better quality of life. What is Urinary Incontinence (UI)? Urinary Incontinence (UI) is a condition where there is an involuntary loss of urine or bladder control causing a person to frequently feel the need to urinate. The severity of UI can range from occasionally leaking urine when you cough or sneeze, to having an urge to urinate that is so sudden and strong where you need to immediately rush to the toilet. These problems, according to Dr Sulaiha, may be caused by various reasons such as damaged pelvic floor muscles during childbirth (particularly if there was difficulty during vaginal child birth), increased pressure in your abdomen due to pregnancy, obesity and prolonged coughing, or neurological conditions that affect the brain and spinal cord such as Parkinson’s disease or multiple sclerosis. A weak or damaged muscles that close up the bladder neck when you feel like urinating, may not be able to stay tightly closed as well. What are the consequences? Women who experience UI might have their daily lives affected as it can be quite embarrassing sometimes. Some find it hard to be out socialising or be physically active when they can’t control the leakage. This may lead to sexual deprivation, hygiene issues and infections. Not only that, UI can be a hindrance when it comes to performing religious rituals such as prayers. All these consequences may lead to depression in individuals who are experiencing this condition. Do I really need to see a doctor? Urinary incontinence can restrict your activities and limit your social interactions. In older adults, rushing to the toilet can increase the risk of falling down. If this problem is affecting your quality of life, it is best to seek professional medical advice from a doctor, or even better, a urogynaecologist. Types of incontinence To understand UI and how to manage it, Dr Sulaiha explained the various types of incontinence and their causes. • Stress Incontinence o Stress here refers to physical and not mental stress. Generally, coughing, sneezing, laughing, heavy lifting, and exercise should not cause any urine leakage. However it could happen in small or large amount if the system to close the bladder during build-up of pressure is not intact. Some could still leak even when the bladder is not full. • Urge Incontinence o This is when you feel a sudden and very intense need to pass urine and you’re unable to delay going to the toilet. Things such as the sound of running water or a change of sitting position could trigger the need to pass urine. Your overactive bladder may cause you to pass urine very frequently at daytime and also at night and this disrupts your routine as well as your sleep. • Mixed Incontinence o Mixed incontinence is when you have symptoms of both stress and urge incontinence. One example is that when you cough or sneeze, you may leak urine and also feel the intense urge to pass urine. • Overflow Incontinence o Overflow incontinence occurs when the bladder cannot completely empty when you pass urine or you lose the sensation of urinating despite the bladder being full. You may experience a frequent or constant dribbling of urine. 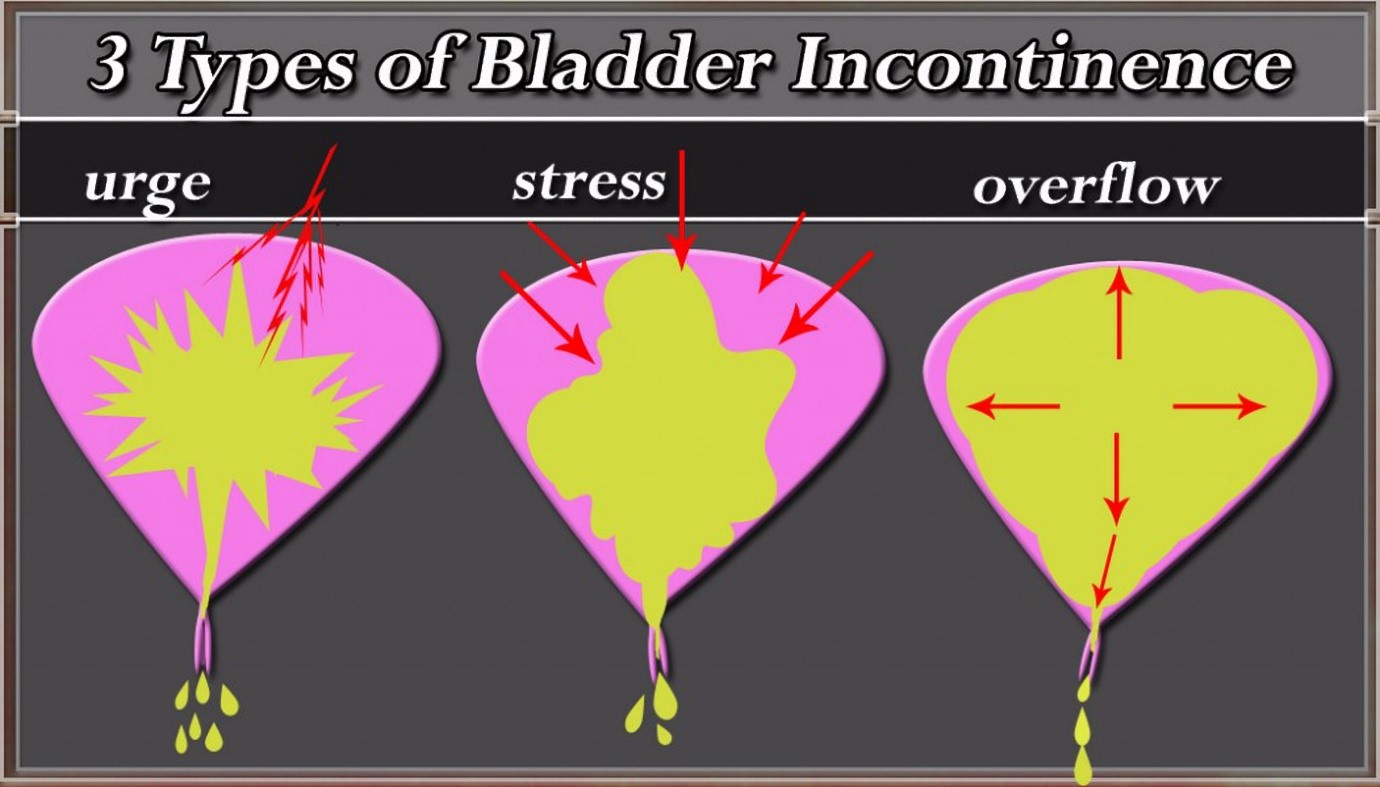
How can UI be treated? The treatment for UI will depend on the type of UI you have and how serious your symptoms are. Here are some types of treatment that your doctor or urogynaecologist might recommend: • Behavioural Therapy o Our thoughts, feelings, and behaviour can affect one another. Keeping a bladder diary where you record what you drink, the time you drink it, the time you urinate and how many times you leak will help when discussing with your doctor how to better control your ‘water work system’. • Medication o There are drugs available to treat UI and it is best to seek your urogynaecologist’s advice. Do bear in mind that while there are benefits in taking medications to help, they do come with side-effects as well. • Surgery o Surgery to correct the anatomical structure definitely might be useful depending on your condition. It is a simple procedure that involves making a small incision in your vagina, insertion of a small graft (material that can be absorbed by your body), fixing it to an appropriate supporting area, lifting up the neck of your bladder to improve its position and function. • Non-surgical method o There are non-surgical methods available where incontinence products can help you manage your UI. Small devices can be placed into the vagina or urethra to prevent urine leakage.
Dr Sulaiha stressed that the most suitable treatment for you would depend on the type of incontinence you have. Whatever it is, your doctor would be able to provide the best recommendation for your specific condition.
Can it be prevented? Dr Sulaiha explained some of the things we can do to prevent it. • Adopt a healthy lifestyle. Diabetes and being overweight are common factors of UI. So it is important to try and be in your ideal weight range by eating healthy and maintaining an active lifestyle. • Avoid lifting heavy weight unnecessarily. Women who may already have weak pelvic floor muscles would worsen it with persistent heavyweight lifting as it increases pressure in your abdomen. They not only may present with UI, prolapse of their vaginal wall could also simultaneously occur, worsening the problem. • Avoid taking highly caffeinated drinks, alcohol and diuretic drugs (medication that increases the need to pass urine). These can irritate the bladder and make you urine more frequently. • Do some bladder training as with other form of training, it could lead to achieving control. In this case, it may allow you to consciously tell yourself whether to hold or if it’s time to go. Typically, our bladder can hold up to 500ml of water before we need to urinate. Women with urge incontinence can find it helpful by lengthening the time between trips to the bathroom. • Get some local hormone application. Women who is menopausal may have problem with vaginal dryness or bladder irritability due to the aging nature of the structures supporting the water work system. Consultation with your doctor is therefore advisable before considering this. • Make pelvic floor exercises (Kegel exercises) a part of your daily routine. o First, find the right muscles. To identify your pelvic floor muscles, stop urination midstream. If you succeed, you’ve found the right muscles. o Next, improve your technique. Tighten your pelvic floor muscles, hold the contraction for five seconds, and then relax for five seconds. Try it four or five times in a row. Work up to keeping the muscles contracted for 10 seconds at a time, relaxing for 10 seconds between contractions. o Keep your focus. For best results, focus on tightening only your pelvic floor muscles. Be careful not to flex the muscles in your abdomen, thighs or buttocks. Breathe freely during the exercises and avoid holding your breath. o Do this for at least 3 sets of 10 repetitions a day with 10 seconds apart. They don’t have to be done all at once. o This is most effective when initiated under the supervision of your doctor or a physiotherapist. 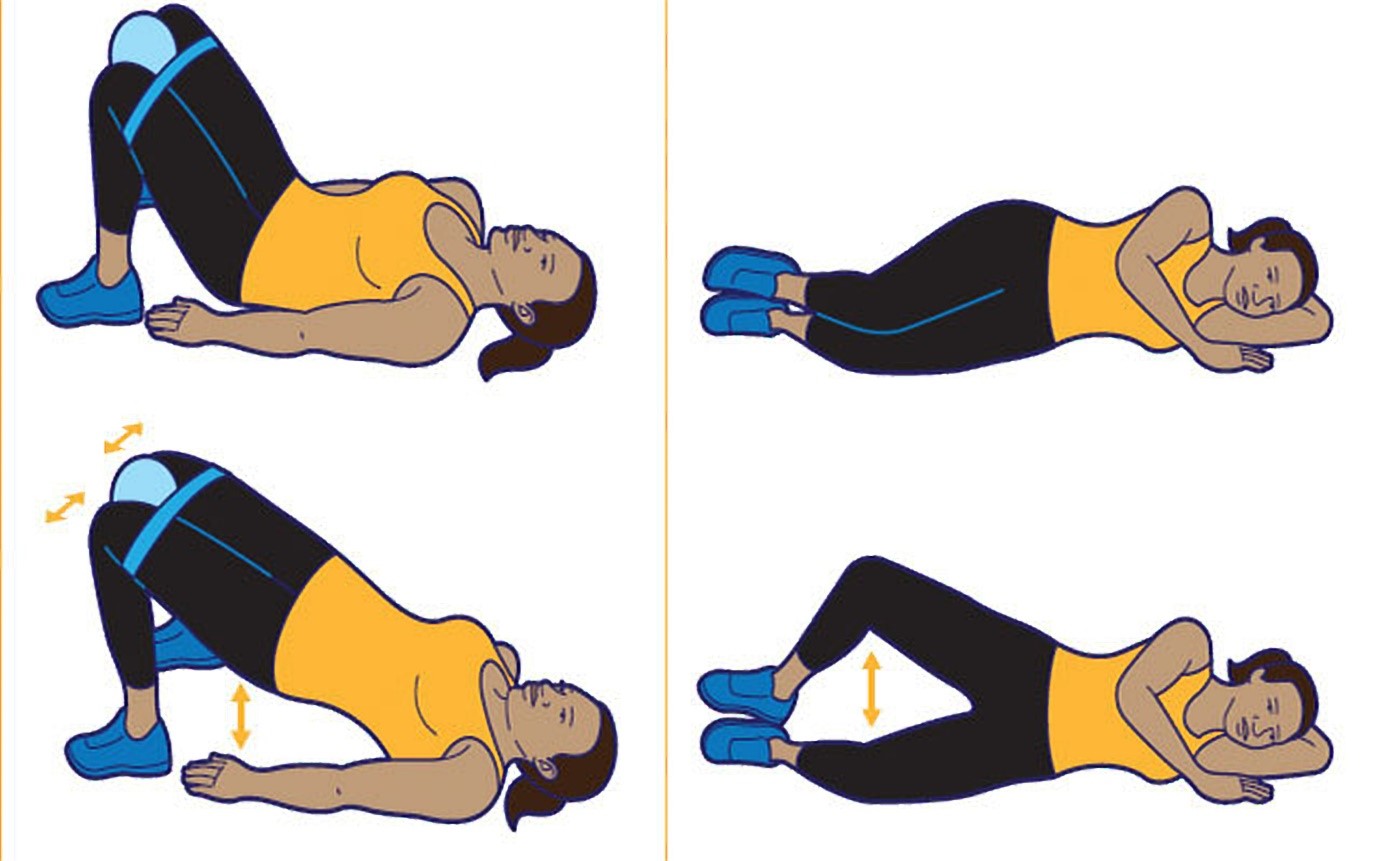
Conclusion
If urinary incontinence is something that affects you in your everyday life, don’t hesitate to see a urogynaecologist.
“You shouldn’t feel embarrassed talking to your doctor about your symptoms. Help is available and can certainly ease your discomfort and to effectively manage the problem. Don’t let UI hinder you from living life to the fullest. The sooner it is treated, the better you’ll feel,” advised Dr Sulaiha.
References: http://www.muacme.org/article.php?aid=588 http://www.mayoclinic.org/diseases-conditions/urinary-incontinence/basics/definition/con-20037883 http://www.nhs.uk/Conditions/Incontinence-urinary/Pages/Introduction.aspx http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/kegel-exercises/art-20045283?pg=1 http://www.augs.org/p/cm/ld/fid=820 This article is brought to you by IMU Healthcare.