Most of us have been prescribed with antibiotics by doctors when we were sick. But do we know what exactly antibiotics do to help us get well? What Antibiotics Do? Bacteria are microorganisms that live all around us and in us. There are good bacteria that are essential to us such as lactobacillus which helps in the digestion of food, and there are bad bacteria that are dangerous and bring us harm such as streptococci which cause inflammation of the tonsils and other infections.
Antibiotics are used primarily to treat bacterial infections. Antibiotics are specific antimicrobial agents that have been used globally for the last 70 years to treat patients who have bacterial diseases such as tuberculosis, syphilis and typhoid. However, because they have been used widely for a long period of time, some common bacteria has – through the course of time – evolved and become resistant to the antibiotics designed to kill them, making the antibiotics less effective. In other words, the bacteria has become antibiotic-resistant, or in broader terms, antimicrobial-resistant. What is Antibiotics Resistance? Antibiotics resistance occurs when certain bacteria change its response when it was repetitively exposed to specific antibiotics at the wrong dosages, wrong duration, wrong timing, wrong indication or worse wrong choice. That certain bacteria, not the persons or animals receiving the antibiotic, become antibiotic-resistant. When we get infected by these changed bacteria again, the infections they caused are harder to treat than those caused by non-resistant bacteria. Think of it as the bacteria wearing a Kevlar protective full-body armour and the antibiotics cannot kill them anymore. Antibiotics resistance is a worrying problem because it leads to higher medical costs, longer hospital stays, and increased mortality. 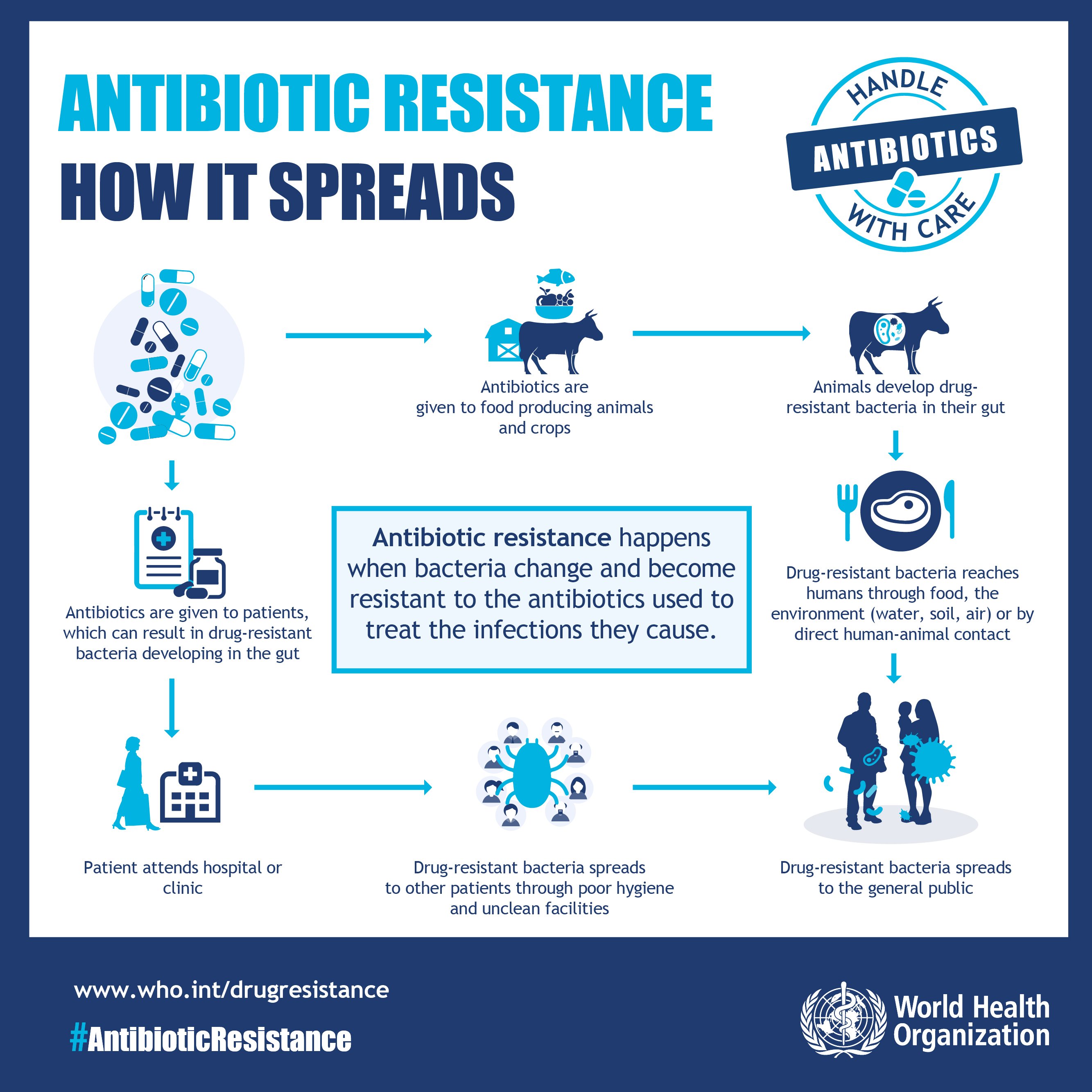 The World Health Organisation (WHO) published a list of bacteria which need new antibiotics recently. The list of antibiotic-resistant “priority pathogens” is made up of 12 families of bacteria that post the greatest threat to human health. Some multidrug resistant bacteria pose a particular threat to hospitals and nursing homes, and they can cause severe and often deadly infections such as bloodstream infections (septicaemia) and pneumonia. How Does Antibiotics Resistance Happen?
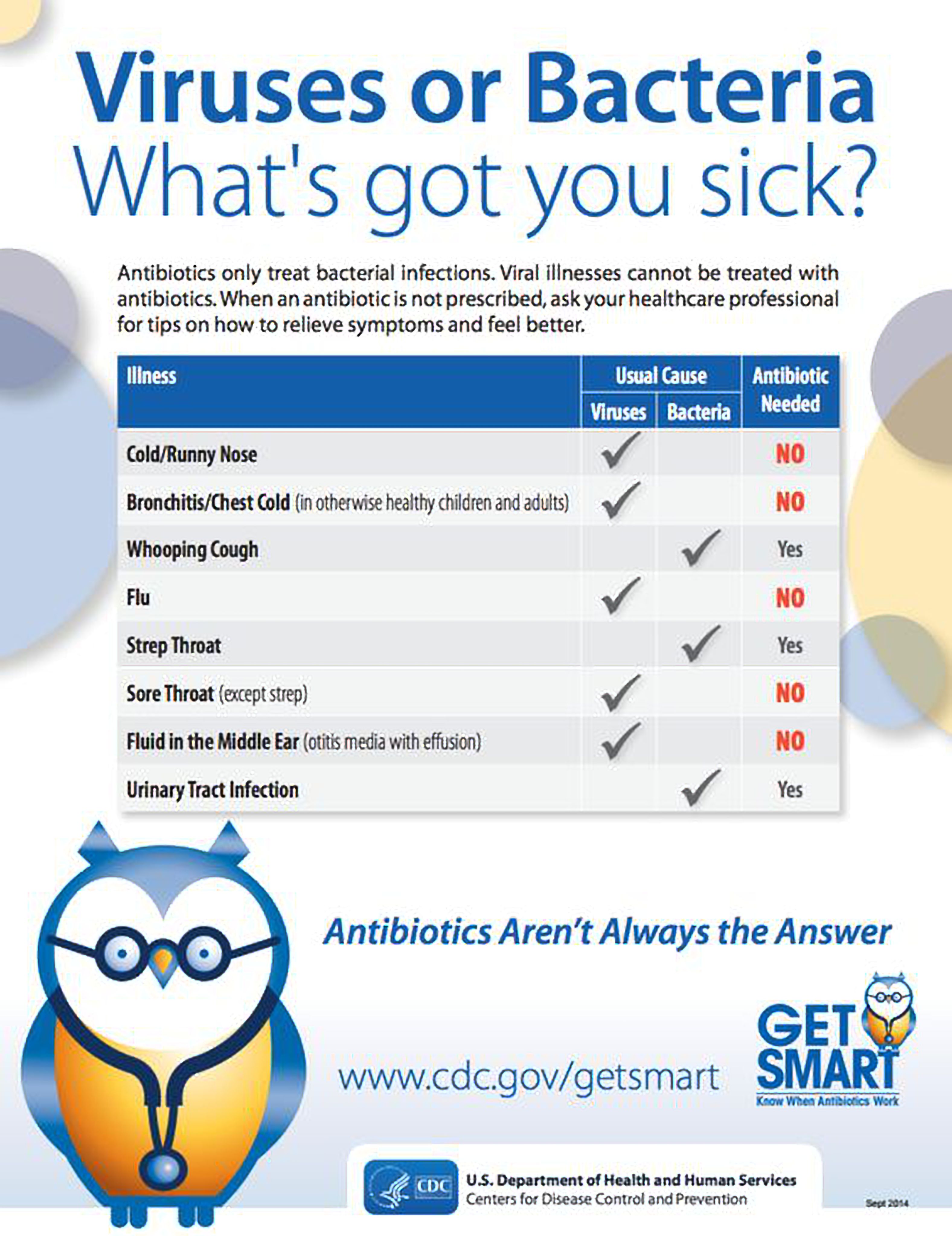
The World Health Organisation (WHO) published a list of bacteria which need new antibiotics recently. The list of antibiotic-resistant “priority pathogens” is made up of 12 families of bacteria that post the greatest threat to human health. Some multidrug resistant bacteria pose a particular threat to hospitals and nursing homes, and they can cause severe and often deadly infections such as bloodstream infections (septicaemia) and pneumonia. How Does Antibiotics Resistance Happen?  Excessive use of antibiotics is the single most important factor leading to antibiotics resistance. The misuse of antibiotics – for example when they are taken by people with common cold (wrong indication) – likewise speeds up this process. This is because a cold is caused by viruses, not bacteria. Furthermore, these antibiotic-resistant bacteria can also be found in people, animals, foods, and the environment (in water, soil, and air). Thus, for example, these bacteria could enter the human body when the meat is consumed. Poor infection control in hospitals and clinic, lack of hygiene and poor sanitation, as well as inappropriate food-handling, will encourage resistant-bacteria to spread. However, according to WHO, since 2011 there is a lack of new antibiotics being developed by pharmaceutical companies to fight resistant-bacteria. This is due to the difficulty in obtaining approval for research and the high cost of research. How Prevalent Is The Problem? According to a study on global antimicrobial resistance rate conducted in 2016, if this situation is left uncontrolled, the number of deaths around the world could go up to 10 million by 2050. Ministry of Health (MoH) Malaysia has established that uncontrolled usage of antibiotics among patients, both prescribed and over-the counter, have increased. In the National Surveillance of Antibiotic Resistance Report 2015, data was obtained from 39 hospital microbiology laboratories and showed that we have almost every variety of antibiotic resistance thus far documented. For instance, the superbug that carries the gene mcr-1 has already been detected in Malaysia which could cause something as simple as urinary tract infection to become life threatening. Malaysians need to be aware and take steps to fight against the spread of antimicrobial resistance. What Can I Do About This? There are many ways to slow down antibiotic resistance. It is crucial to know what the exact causes of infections are and be educated on the right way to use antibiotics. Here are some steps all of us can take: • Use antibiotics only when it is absolutely necessary o Only take antibiotics that are prescribed by a certified health professional for your specific condition. And only if necessary so that the dangerous bacteria in your body do not become resistant. Speak to your doctor if you are unsure. o In Malaysia, one can easily buy antibiotics from retail pharmacies without a prescription. Do not self-medicate or self-prescribed yourself with antibiotics. Consult your family doctor first. Pharmacists and the sales persons at the retail pharmacies are not professionally trained to diagnose infections and prescribe antibiotics.
Excessive use of antibiotics is the single most important factor leading to antibiotics resistance. The misuse of antibiotics – for example when they are taken by people with common cold (wrong indication) – likewise speeds up this process. This is because a cold is caused by viruses, not bacteria. Furthermore, these antibiotic-resistant bacteria can also be found in people, animals, foods, and the environment (in water, soil, and air). Thus, for example, these bacteria could enter the human body when the meat is consumed. Poor infection control in hospitals and clinic, lack of hygiene and poor sanitation, as well as inappropriate food-handling, will encourage resistant-bacteria to spread. However, according to WHO, since 2011 there is a lack of new antibiotics being developed by pharmaceutical companies to fight resistant-bacteria. This is due to the difficulty in obtaining approval for research and the high cost of research. How Prevalent Is The Problem? According to a study on global antimicrobial resistance rate conducted in 2016, if this situation is left uncontrolled, the number of deaths around the world could go up to 10 million by 2050. Ministry of Health (MoH) Malaysia has established that uncontrolled usage of antibiotics among patients, both prescribed and over-the counter, have increased. In the National Surveillance of Antibiotic Resistance Report 2015, data was obtained from 39 hospital microbiology laboratories and showed that we have almost every variety of antibiotic resistance thus far documented. For instance, the superbug that carries the gene mcr-1 has already been detected in Malaysia which could cause something as simple as urinary tract infection to become life threatening. Malaysians need to be aware and take steps to fight against the spread of antimicrobial resistance. What Can I Do About This? There are many ways to slow down antibiotic resistance. It is crucial to know what the exact causes of infections are and be educated on the right way to use antibiotics. Here are some steps all of us can take: • Use antibiotics only when it is absolutely necessary o Only take antibiotics that are prescribed by a certified health professional for your specific condition. And only if necessary so that the dangerous bacteria in your body do not become resistant. Speak to your doctor if you are unsure. o In Malaysia, one can easily buy antibiotics from retail pharmacies without a prescription. Do not self-medicate or self-prescribed yourself with antibiotics. Consult your family doctor first. Pharmacists and the sales persons at the retail pharmacies are not professionally trained to diagnose infections and prescribe antibiotics.
• Always take the full prescription even if you feel better o Many times we have been told to finish our antibiotic over a certain number of days. A lot of research have been done globally to determine the exact dosages and sufficient durations of antibiotics are needed to completely kill and eradicate different types of bacteria. If you stop treatment prematurely, there is a risk the antibiotics have not killed all the bacteria that made you sick. These residual bacteria in your body could evolve and become resistant to the bacteria it has been exposed. • Never use left-over antibiotics and never share antibiotics with others o The obvious reason is its expiry date. Of course, never share your antibiotics with others even if they have been diagnosed with the same illness as the dose prescribed may not be right for them or there may be potential allergic reaction to the antibiotic that they might not be aware of. • Prevent infections by regularly washing your hands, avoiding contact with sick people and keeping your vaccinations up to date. o Hand washing, according to WHO, can prevent up to 30% diarrhoea-related infections and 20% respiratory infections. On top of this, consult your doctor and check if your vaccinations are up to date.  Effective and appropriate use of antibiotics as well as better prevention of infections will be the first major step to address the problem of antibiotic resistance. More research and development is vital, and when new antibiotics are developed in the future, we must remember to use them rationally. References: http://www.who.int/mediacentre/factsheets/antibiotic-resistance/en/ https://www.cdc.gov/drugresistance/ http://www.who.int/mediacentre/news/releases/2017/bacteria-antibiotics-needed/en/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/ https://amr-review.org Review on Antimicrobial Resistance http://www.nst.com.my/news/2016/11/189191/abuse-antibiotics-malaysia-rise-says-health-ministry http://www.imr.gov.my National Antibiotic Resistance Surveillance Report 2015 http://www.thestar.com.my/opinion/letters/2016/09/27/hotbed-of-antibiotic-resistance/ http://www.nhs.uk/conditions/Antibiotics-penicillins/Pages/Introduction.aspx http://www.who.int/features/qa/stopping-antibiotic-treatment/en/ https://www.cdc.gov/handwashing/why-handwashing.html This article is brought to you by IMU Healthcare.
Effective and appropriate use of antibiotics as well as better prevention of infections will be the first major step to address the problem of antibiotic resistance. More research and development is vital, and when new antibiotics are developed in the future, we must remember to use them rationally. References: http://www.who.int/mediacentre/factsheets/antibiotic-resistance/en/ https://www.cdc.gov/drugresistance/ http://www.who.int/mediacentre/news/releases/2017/bacteria-antibiotics-needed/en/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/ https://amr-review.org Review on Antimicrobial Resistance http://www.nst.com.my/news/2016/11/189191/abuse-antibiotics-malaysia-rise-says-health-ministry http://www.imr.gov.my National Antibiotic Resistance Surveillance Report 2015 http://www.thestar.com.my/opinion/letters/2016/09/27/hotbed-of-antibiotic-resistance/ http://www.nhs.uk/conditions/Antibiotics-penicillins/Pages/Introduction.aspx http://www.who.int/features/qa/stopping-antibiotic-treatment/en/ https://www.cdc.gov/handwashing/why-handwashing.html This article is brought to you by IMU Healthcare.











Ming Gopie
Greate article. Keep posting such kind of information on your site. Im really impressed by it.